Is consuming expired prescription medicines really all that dangerous? Some friends of mine insist taking pills beyond the printed expiration date is flirting with death, while another claims expiration dates on labels are BS, there solely to prompt us to order refills and spend more money. I once treated a nasty headache with the only thing I had on hand, some Vicodin that was about a year out of date. My headache went away, and I was no worse for wear. As time passes, are the pills in their little plastic bottles chemically restructuring themselves into poisons, or is there nothing to fear? —Neil, Indiana
We have to tread carefully here, Neil. A few drugs don’t age well—for example, nitroglycerin and insulin. But they’re the exception. Most drugs retain their potency for years after they supposedly expire. What’s more, everybody knows this, or ought to; The Wall Street Journal once ran a front-page exposé on the subject.
But you don’t see anyone pushing for expiration-date reform. Why not? No doubt because of the same combination of greed and excessive caution that drives up all health-care costs: 1. The drug companies potentially could forego billions of dollars in lost sales; 2. The amount individual consumers could save is relatively trifling; and 3. There’s a remote but nonzero chance somebody relying on defunct drugs could die.
This last belief is based partly on a 1963 study claiming expired tetracycline had caused kidney damage. But that contention has been questioned, and in any case, the problematic formulation of tetracycline is no longer made.
The FDA started requiring drug companies to place expiration dates on drugs in 1978 on the reasonable grounds that people shouldn’t be using medicine so old it was no longer safe or effective. What the FDA didn’t do was set expiration dates, leaving that up to manufacturers. In 1985, the U.S. Pharmacopeia, a nonprofit standards-setting body, began urging that medicines not sold in the manufacturer’s original container (that is, most medicines dispensed by pharmacists) have a one-year expiration date. The theory was that pharmacy pill bottles left in the notoriously hostile environment of your medicine cabinet (or, to be fair, a hot glove compartment) were less likely to prevent their contents from going bad.
But the truth is your meds will probably keep just fine. In the mid-’80s, the FDA started testing drugs as part of the U.S. military’s Shelf Life Extension Program—the Pentagon then had a $1 billion stockpile of drugs it didn’t feel like throwing out. As reported in that Wall Street Journal article in 2000, around 90 percent of the drugs were safe and effective well after they’d nominally expired.
To be sure, some drugs deteriorate faster than others. For example, epinephrine, used to treat cardiac arrest, steadily loses its potency over time. Liquid drugs and suspensions are less stable than solids. Medications custom-prepared by your local pharmacy are likely to have a short shelf life.
But even then, it’s not like drugs go bad at the stroke of midnight. An update on the Shelf Life program published in 2009 established that 88 percent of tested medications worked fine more than five years past their expiration date, which admittedly just confirmed previous research. The more pertinent finding from a practical standpoint was this: One year post-expiration, every drug tested was still OK.
Word has been gradually filtering out. In the January 2012 Consumer Reports, the magazine’s chief medical adviser, Marvin Lipman, writes, “Except for tetracycline”—and as we’ve seen, even that’s dubious—“expired drugs generally don’t appear to cause harm. But they do become less potent. In particular, throw out any drug more than a year past its expiration date [my emphasis].”
But let’s face it, not everybody reads Consumer Reports. And some drugs are good for much longer. What’s needed is a systematic revamping of drug-expiration labeling so the dates reflect the actual length of time, based on tests, that particular medicines retain their potency.
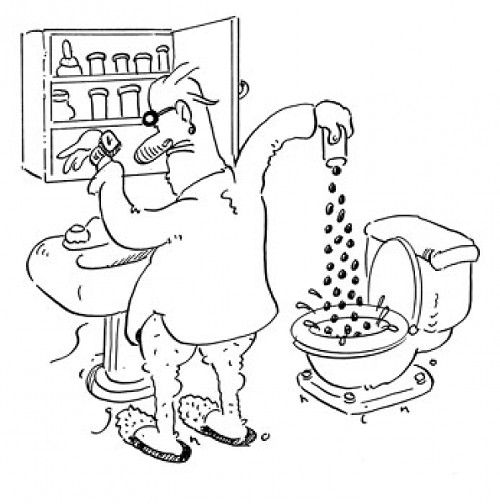
The savings could be huge. From 1993 to 1998, the military spent $4 million testing expired medicines and saved $263 million. A follow-up study found that for every dollar spent on the Shelf Life program from 2006 to 2010, $10 to $20 was saved. In 2010, Americans spent $307 billion on four billion prescriptions, nearly double what they’d laid out 10 years earlier. In one survey, only 2 percent of respondents said they used all their medication before it expired. (And more than a third flushed expired medications down the toilet, wreaking who knows what environmental havoc.) Even a small extension of expiration dates could save billions.
As we’ve seen, however, neither the drug industry nor consumers have much incentive to demand change. Some outside crusader, maybe? Not likely. Suppose you announce you’re campaigning for office on a platform of prodding the pharmaceutical industry to push back expiration dates. Next day, guaranteed, there’ll be billboards all over town saying “MY OPPONENT WANTS TO SELL YOU STALE DRUGS.”
Send questions to Cecil via StraightDope.com or write him c/o Chicago Reader, 11 E. Illinois, Chicago 60611. Subscribe to the Straight Dope podcast at the iTunes Store.
More by Cecil Adams
-
This Is the End, My Friend
This week's Straight Dope marks the last appearance of the column as the Teeming Millions have known it for the past 45 years.
- Jul 11, 2018
-
Do Brain Supplements Do Anything?
Brain Drain
- Jul 4, 2018
-
Is flying really worse for the environment than driving?
Planes and Trains
- Jun 27, 2018
- More »