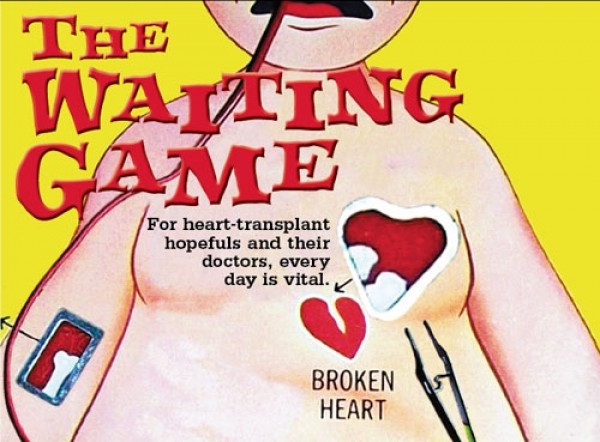
The Waiting Game
For heart transplant hopefuls and their doctors, every day is vital
By Courtney TannerDeborah Budge won’t tell you what’s on her grocery list or what her deepest fears are. She won’t talk about her favorite memory or her personal life.
No, Budge does not wear her heart on her sleeve. And her sleeves themselves are covered by the polyester-blend white lab coat she wears every day to work as a cardiologist at Murray’s Intermountain Heart Institute.
What Budge will talk about is her devotion to her job and her belief in its importance. The 37-year-old, who joined the staff of Intermountain Medical Center in 2009, has been part of more than 200 heart transplants during her training and career. For Budge, these numbers are what make up her life. They represent her accomplishments and failures.
“To me, there’s nothing greater than to take somebody that has heart failure to such a degree that they’re incredibly limited and have a short life expectancy and to be able to give them a completely new life,” she says.
But Budge’s impact on those patients goes beyond the physical recuperation. And no two patients know Budge’s personal form of medication better than Dylan Peterson and Mike Mader.
Peterson, who received a heart transplant in June 2010, has worked with Budge constantly since his surgery for check-ups on his heart and speaks warmly of Budge and her sincerity.
“She’ll tell you what’s going on, but she takes more of a motherly approach,” Peterson says. “She tells it to you nicely.”
Mader met Budge in 2010 when he was assigned to her heart-failure group after having more than 18 heart attacks. He received care under Budge’s supervision for nearly three years. After 718 days waiting on the transplant list, he had a combined heart and liver transplant in April 2013. It was the first combined procedure in the Intermountain Region.
“It was always a relief to see Budge,” Mader says. “She’s an incredible person. And I feel extremely fortunate to have had her be a part of my care.”
Mader has continued to have a “good open relationship” with Budge as his doctor. He says her ability to look beyond his heart issues and genuinely care about his personal life made a difference in his medical care.
Both men say if it weren’t for Budge, their stories might not have had happy endings.
And even with a transplant, the health challenges facing heart transplant patients are far from over. Both Mader and Peterson face a lifetime of medication and doctor visits. Still, both men say the checkups are a worthy tradeoff for the uncertainty and gravity of the organ-donor waitlist.
Intermountain Donors Services, Intermountain Medical Center’s partnership for coordinating donations, estimates that the waiting list for a heart transplant is usually at about 50 people. The need outpaces the available organs by more than 25 percent; roughly 35 heart transplants are done in Utah each year, leaving many in limbo.
“There are definitely people who die every day waiting for organs,” Budge says.
The Tin Man
Peterson was running toward first base during a 2007 varsity baseball game when he suddenly blacked out.
Peterson’s parents took the Richfield High School senior to the hospital, where doctors confirmed heart failure. He had a ventricular arrhythmia—an abnormal rhythm in the bottom of the heart, which can cause blackouts and sometimes results in death.
It was not a total bolt from the blue. Peterson had been born with a weak heart; at birth, he was diagnosed with idiopathic cardiomyopathy—a weakness of the heart muscle with an unknown origin. It occurs in children younger than 18 in just 1.13 cases out of 100,000.
For 18 years, Peterson had been able to control his condition with medication.
“My heart wasn’t perfect, but it was enough to get by,” Peterson says. “But they realized they wouldn’t be able to stall it forever with medication.”
And now he was in heart failure, where the heart does not pump an adequate amount of blood to support the body.
So doctors put Peterson on the waiting list for a heart transplant.
A few months later, doctors implanted a defibrillator, a special kind of pacemaker, in Peterson’s chest to help in the meantime. It would deliver a shock when his heart experienced anomalous rhythms, like those that caused Peterson to black out.
But despite the defibrillator, Peterson’s abnormal heart rhythms were becoming more frequent. And the longer he waited for a transplant, the higher his risk of sudden death.
On Oct. 24, 2009, Peterson went into cardiac arrest. His defibrillator shocked him 12 times before he reached Intermountain Medical Center, where his heart rate reached 220 beats per minute. He did not leave the hospital after that for nine months.
“He was not going to be stable to just wait for a heart,” says Budge, who worked closely with Peterson during those months.
Less than two weeks later, on Nov. 3, doctors implanted the Total Artificial Heart in Peterson.
Though heart transplants are rare enough, Total Artificial Heart transplants are far more uncommon. On average, there are only 20 patients with the Total Artificial Heart each year across the United States. The two artificial-heart machines available at Intermountain Medical Center are used just once every one or two years. Intermountain Medical Center and its sister hospital, LDS Hospital, have implanted just 13 Total Artificial Hearts in two decades since the Artificial Heart Program began in 1993.
“The heart is the most important organ, so to think that it can be removed and completely taken over by a machine is pretty incredible,” Budge says.
And Peterson’s wait was longer than most. He stands at 6 feet, 9 inches tall, and had to find a heart big enough to support his body.
He was on the transplant list for 681 days; 227 of those days were spent waiting in the hospital.
The time in the hospital attached to the artificial heart machine did not move quickly for Peterson. And it became even more psychologically taxing than it was physically.
“After about the third or fourth month, I realized it was going to take a while for [a heart] to come,” Peterson says. “Every day ... I was hoping something would happen, and then night would come and I wouldn’t have a heart.”
To pass the time, Peterson played video games like Call of Duty online with friends. While he pumped lead into virtual soldiers, the 450-pound artificial heart machine kept his heart pumping with tubes running out of the left side of his abdomen. He nicknamed the machine Big Bertha; he constantly heard its hum and could feel as it expanded his chest to keep his heartbeat stable.
“It kept my heart rate constantly at 140 beats per minute—well, I don’t know if it’s a heart rate; I only had part of a heart,” Peterson says jokingly. But, he says, it was “a comfort knowing that, for the most part, the artificial heart wouldn’t stop beating; I could always trust on it.”
But by June 2010, Peterson’s disposition started to contrast with the weather outside the hospital. As the sun became brighter, he became gloomier. He had been on the artificial-heart machine for 227 days, and he was tired of waiting.
On June 18, Peterson, convinced his stay at the hospital was infinite, was planning to ask his doctor, Rami Alharethi, if he could switch medications so he could stop lugging around a drug drip pole in addition to Big Bertha. He wanted to exchange his intravenous blood thinner Heparin for a pill, Coumadin. Most doctors do not prescribe Coumadin to patients waiting for a heart transplant; it has a longer half-life and can linger in the blood for more time, and excessive blood thinners can cause issues in surgery. But Peterson, who had begun to lose hope for a new heart, was willing to make the change.
Then, at 9 a.m., Alharethi entered Peterson’s room to tell him that he had a donor heart. It was just another 10 hours before Peterson went into the operating room for his transplant; eight hours later, he was out again.
But for Peterson, “time wasn’t moving fast enough. I wanted that heart and I wanted to start my life again.”
More by Courtney Tanner
-
The Lumineers at Great Saltair
- Sep 18, 2013
-
Glad You Asked: SL Bees, Spider-Man, Huey Lewis and the News
- Jul 23, 2013
-
Glad You Asked: '80s Insanity, Belle & Sebastian, SL Bees
- Jul 18, 2013
- More »
Latest in Cover Story
Readers also liked…
-
Forget the family pedigree—Robert F. Kennedy Jr should not be the next president of the United States
Trojan Horse
- Jun 21, 2023
-
Women decry harassment and toxic culture at St. George auto dealership
Men at Work
- Oct 11, 2023